Killing Germs With UV-C Light
The latest cleaning technologies, tools, and products have made “cleaning for health” a reality for industry professionals. These technologies have advanced since the early 1900s, when an understanding on how to disinfect drinking water with chlorine helped control and end many diseases, such as typhoid fever, which is caused by salmonella bacteria. Since then, we’ve created vaccines and medicines for respiratory viruses, which continue to impact the daily lives of people around the world.
As we enter 2024, facility managers and cleaning professionals continue to face challenges in eliminating infectious, disease-causing germs from the built environment while staying within their budgets. These germs can spread directly from person to person, indirectly through the air as small droplets or tiny aerosol particles, or through high-touch surfaces that have been contaminated by pathogens from the air or from a person who is sick.
Indoor air quality (IAQ) strongly impacts respiratory health. The cleaning industry plays an essential role in reducing the transmission of respiratory diseases through the improvement of IAQ.
Today, more tools are available to fight respiratory infections, including both nonchemical and chemical-based cleaning and disinfection; air filters and purifiers; ventilation, filtration, and increased air exchange through HVAC system improvements; and ultraviolet (UV-C) light systems. Through ISSA’s GBAC STAR facility accreditation program, we are seeing facility managers take a more evidence-based and systematic approach to reducing the risk of infectious disease spread inside their buildings by implementing a layered approach to cleaning and disinfection, which is the strategy recommended by the Global Biorisk Advisory Council® (GBAC), a Division of ISSA.
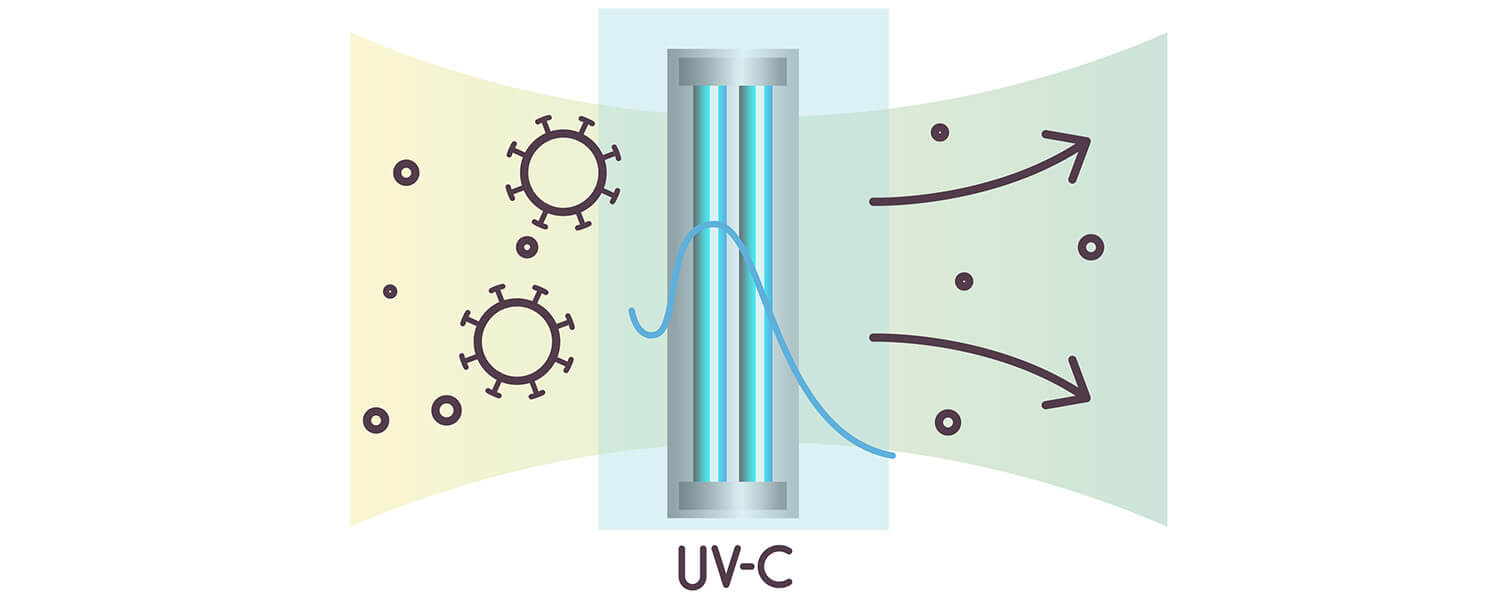
Germicidal ultraviolet light (UV-C) technology, specifically, can be effective in many indoor spaces and is especially useful as an additional layer of protection to reduce infectious germs.
UV-C light disinfection is growing in popularity. The global UV-C disinfection equipment market was valued at US$1.3 billion in 2019 and is projected to reach $5.7 billion by 2027, growing at a compound annual growth rate (CAGR) of 17.1% from 2020 to 2027, according to Allied Market Research.
CMM reached out to Doug Hoffman, the executive director of the National Organization of Remediators and Microbial Inspectors (NORMI™), and Dr. Gavin Macgregor-Skinner, senior director of GBAC, to learn how UV-C can be an effective tool against infectious airborne diseases.
What’s the problem with current IAQ standards?
Dr. Gavin Macgregor-Skinner
Current IAQ standards do not consider infectious disease risk and include airborne pathogen levels. Very few buildings measure their indoor air quality, even though indoor air quality monitors are available and affordable. There’s a lack of standards, education, and training on the implementation and costs of deploying a layered approach to improve IAQ.
Doug Hoffman
We need to implement a layered approach and mass deployment of IAQ interventions that include ventilation, filtration, air ionization, photocatalytic oxidation (PCO, which is explained further in the Q&A), and ultraviolet germicidal irradiation (UVGI). We have training on effective interventions to improve IAQ, and we have tools to measure it as well.
How does UV-C light disinfection work?
Macgregor-Skinner
UV-C radiation is a known disinfectant for air, water, and nonporous surfaces. It has effectively been used for decades to reduce the spread of bacteria, such as tuberculosis. For this reason, UV-C lamps are often called “germicidal” lamps. UV-C radiation eliminates the outer protein coating of bacteria and viruses, ultimately leading to the inactivation of the microorganism.
Hoffman
UV-C light’s efficacy is dependent upon the organic load and microorganisms, the intensity and time of exposure, the distance from the surface, and whether the surface is within a direct line of sight. UV-C light can only inactivate a germ if the germ is directly exposed to the light. UV-C light requires a sufficient duration of exposure to be effective, and this can vary for different microorganisms—bacteria, viruses, fungi.
What is the correlation between wavelengths and germicidal irradiation?
Hoffman
Humans can see visible light as waves of electromagnetic radiation between about 400 to 700 nanometers (nm). A nanometer is one millionth the size of a millimeter. Radiation with wavelengths just longer than visible light is called infrared, and longer radiation wavelengths than this are radio waves. Radiation with wavelengths just shorter than visible light is called ultraviolet; shorter radiation wavelengths than this are X-rays. Ultraviolet (UV) light is subdivided into UV-A (315–400 nm), UV-B (280–315 nm), and UV-C (100–280 nm). UV-C is effective at killing a wide range of microorganisms, including viruses. When a light looks like UV (like a blacklight), it might not be at a wavelength that can kill or deactivate microbes. The only way to know for sure that you are using the right UV-C light is to find the wavelength the light is generating. The manufacturer, of course, will provide that information.
Macgregor-Skinner
The UV-C disinfecting process, UVGI, uses short-wavelength UV (200–280 nm) light to kill or inactivate microorganisms by disrupting their genetic material (DNA or RNA), leaving them unable to perform vital cellular functions, resulting in cell death. The Tuberculosis Ultraviolet Shelter Study, conducted at 14 homeless shelters in six U.S. cities from 1997– 2004, found that UV-C lights placed at least 6.9 feet above the floor could disinfect the air and were safe for humans with no increase in the most common side effects of accidental UV-C exposure.
Where can you put UV-C lights in the built environment?
Hoffman
UV-C technology can be installed in HVAC systems, packaged terminal air conditioners (PTACs), heating systems, fresh-air makeup devices, and other air-conditioning equipment to address the air in any environment. However, not all the air invariably gets to those devices, so having this technology in standalone units is sometimes the best option. A combination of technologies is a wise choice for those who use their air conditioning and heating systems sporadically.
Macgregor-Skinner
GBAC STAR-accredited facilities, including airports, hospitals, hotels, nursing homes, office buildings, schools, and stadiums, have made significant improvements by implementing a layered approach to improving IAQ. Indoor air safety begins with ventilation, but it usually can’t end there. It also can include filtration, using high-efficiency particulate air (HEPA) filters, along with UVGI lamps that use UV-C to kill viral, bacterial, and fungal organisms. Trained professionals install these lamps, which primarily use 254 nm wavelengths, high up in a room. Far-UVC lamps use primarily 222 nm wavelengths and can be set up in a room without professional installation. Airborne germs are killed once they receive an appropriate amount of UV energy. The particles remain in the air or land on surfaces, but they are no longer infectious.
Where are the most important locations for UV-C lights?
Macgregor-Skinner
The most important locations are high-risk indoor settings—spaces where there is an increased likelihood of people showing systems of illness, such as hotels, airports, and any crowded buildings, especially when the health status of the facility inhabitants are unknown.
Hoffman
UV-C technology should be deployed in rooms with insufficient or no mechanical HVAC systems and where adequate ventilation cannot be maintained year-round. Rooms should have a minimum ceiling height of at least 8 feet and some airflow, such as fans at low speed. UV-C lights are not necessary in outdoor open-air seating areas.
What types of UV-C devices are available for indoor air and surfaces?
Macgregor-Skinner
The market has increased significantly. GBAC STAR-accredited facilities are currently implementing the following UV light disinfection systems:
- Upper-Room UVGI: These systems are installed above people’s heads on walls or ceilings (usually at least 7 feet from the floor).
- HVAC UV Systems: These are integrated into the building’s HVAC systems and may include advanced components to provide technologies like PCO and additional ionization.
- Mobile UV Units: These portable UV systems can be moved from room to room for targeted disinfection.
- Handheld UV Devices: These small, portable devices provide spot disinfection for surfaces like handrails, keyboards, elevator buttons, doorknobs, furniture, and other hard-to-clean areas. They require proper safety precautions to avoid direct exposure to skin or eyes.
- Direct UV-C Surface Disinfection Lamps: These lamps are designed to be placed in a room to irradiate surfaces directly with UV-C light.
- UV-C Conveyor Systems: Used in industrial or commercial settings, these systems disinfect equipment, tools, or products moving along a conveyor belt.
- Robotic UV Disinfection Systems: These systems can navigate around rooms autonomously.
Hoffman
Not all UV-C lamps are equal. Some might emit definitively specific wavelengths or a broad range of wavelengths. The ability to choose the correct design and size of effective UV-C light systems requires specific knowledge and experience. Seek consultation with a reputable manufacturer or a well-trained, experienced IAQ professional prior to purchasing and installing.
Is UV-C exposure time a factor in its effectiveness?
Hoffman
Commonly called “dwell time” or “contact time” when speaking about chemicals, exposure time is an important factor when using UV-C. The microbes must be exposed to the UV-C long enough to damage the microbe. In our NORMI classes, I make the point that in the HVAC system, when the microbes pass by the UV-C lamp more than 500 cubic feet per minute (cfm), the microbes are not even getting “sunburned.” UV-C is very effective when proximity and exposure time are taken into consideration. When ignored, the UV-C light might make folks feel better about the environment, but they are just functioning as pretty lights.
Can UV-C systems replace the need for standard cleaning processes?
Hoffman
In the cleaning process, there are very few, if any, techniques that replace the need to mechanically remove the contaminants. If the microbes are covered by a coat of dust, they will not be exposed to the UV-C and, therefore, not exposed to its germicidal wavelength.
Are there other technologies that can work with UV-C lights?
Hoffman
In the 1990s, engineers learned that placing a target plate, covered with a metallic coating, close to the UV-C lamp would produce oxidizers that traveled downstream through ductwork and disrupted microbes on surfaces and in the air. This technology, dubbed photocatalytic oxidation (PCO), was first introduced using UV-C at a wavelength that would produce ozone. As the technology evolved, the addition of ionization—like the dielectric barrier ionizer—enhanced the power of the PCO technology and resulted in efficacious air and surface purification without the use of ozone. A large volume of testing data from both clinical and field settings proves the safety for humans and efficacy of this technology against fungi, bacteria, and viruses in the built environment. This is a good example of a multi-strategic approach to a multi-faceted problem that is fast becoming a solution to help keep air and surfaces cleaner.
Are there any safety considerations for using UV-C devices?
Macgregor-Skinner
When using UV-C lights for surface and air disinfection, you must consider health and safety factors, as well as the risk of incomplete inactivation of bacteria and viruses.
It’s important to follow safety guidelines to protect against harmful UV-C exposure. Additionally, the effectiveness of UV devices can vary based on the intensity of the UV-C light, the duration of exposure, and the type of pathogen being targeted.
Warning labels are not enough. Remember that UV-C disrupts DNA. Unsafe levels of UV-C radiation can cause injury to the skin (erythema, a burn-like skin reaction) and eyes (photokeratitis) after a few seconds of exposure. Never look directly at a UV-C lamp source, even briefly. There are no immediate warning symptoms to indicate overexposure to UV-C radiation.
Hoffman
The best UV-C devices provide a shield, or the lamp itself is installed in such a way as to make it difficult for anyone to look directly at the light. Those shields may take the form of a honeycomb or other shape to obscure the lamp. Another concern is ozone. Depending on design, power, and operation time, UV-C lamps below 240 nm can generate ozone. However, many people harbor misunderstandings about the actual generation and dissipation of ozone molecules by UV-C lamps. Unmonitored ozone itself is hazardous, and it also interacts with volatile organic compounds (VOCs) to create particulate matter in the air. IAQ monitors can measure ozone and particulate pollution.
A study in Baltimore, Maryland, found that although Far-UVC 222nm light in a standard hotel room increased ozone concentrations, the indoor ozone levels remained lower than those outdoors and well below U.S. Environmental Protection Agency (EPA) ambient limits and those of the U.S. Occupational Safety and Health Administration (OSHA) of 0.10 parts per million (ppm) for eight hours. UV-C 254 nm light does not generate ozone.
How do I learn more about UV-C light disinfection devices?
Macgregor-Skinner
As with any cleaning system, training and support on UV-C is critical. To learn more, you should:
- Ask for education and training opportunities.
- Ask the manufacturer about the device’s health and safety risks.
- Ensure you understand the instructions for installation, use, cleaning, and maintenance.
- Test the lamp to determine whether it puts out other wavelengths.
- Ask which surfaces are compatible with UV-C disinfection.
- Ask whether the device generates ozone.
Ask whether the lamp contains mercury. (If the lamp is damaged, you will need this information to clean up and dispose of the debris safely.)
Doug Hoffman is the founder and executive director of NORMI™, the National Organization of Remediators and Microbial Inspectors (www. normi.org), a not-for-profit training and certification organization for IAQ professionals. His passion is helping people understand how to live healthier lives indoors and empowering them with the ability to have cleaner air.
Dr. Gavin Macgregor-Skinner is the Senior Director of the Global Biorisk Advisory Council® (GBAC), a Division of ISSA. As an infection prevention expert, epidemiologist, and university professor, he works to develop protocols and education for the global cleaning industry to empower facilities, businesses, and cleaning professionals to create safe and healthy environments.